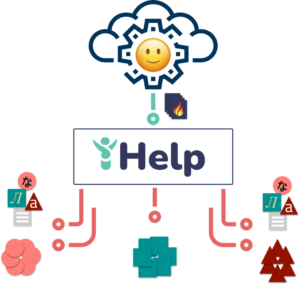
The iHelp project aims at early identifying and mitigating the risks associated with Pancreatic Cancer by applying advanced AI-based learning and decision support techniques on the historic (primary) data of Cancer patients, integrated with (secondary) data gathered through the mobile and wearable applications (concerning lifestyle, behavioural, social interactions and response to targeted prevention and intervention measures).
Despite the increasing recognition of the importance and potential benefits of interoperability for patients and health systems, implementing truly interoperable health ecosystems remains a considerable challenge for a number of reasons including heterogeneous data formats across systems, clinical information complexity, knowledge specific to certain medical specialities, clinical context, over-complexity of standards, the lack of shared-meaning and misunderstandings between system suppliers and end-users.
 The present-day health data ecosystem comprehends a wide range of complex heterogeneous data sources. Health-related data is currently being produced, collected and stored in various formats across multiple types of systems. In addition to typical medical systems at hospitals, medical centres and health organisations, new ICT services (e.g., that use IoT devices, sensors and mobile applications for health monitoring or decision support) also collect a vast amount of health-related data. Currently, all these systems operate independently: data exists either as free-text or structured data, that may be organised in a proprietary way or be coded using one-of-many coding, classification or terminologies that have often evolved in isolation and designed to meet the needs of the context that they have been developed in. For example, data about medical conditions and medical tests are typically kept at the hospital, data about physical fitness and wellbeing is captured by wearables and mobile apps and stored by 3rd party platforms and data about eyesight and dental problems is stored separately in specific systems.
The present-day health data ecosystem comprehends a wide range of complex heterogeneous data sources. Health-related data is currently being produced, collected and stored in various formats across multiple types of systems. In addition to typical medical systems at hospitals, medical centres and health organisations, new ICT services (e.g., that use IoT devices, sensors and mobile applications for health monitoring or decision support) also collect a vast amount of health-related data. Currently, all these systems operate independently: data exists either as free-text or structured data, that may be organised in a proprietary way or be coded using one-of-many coding, classification or terminologies that have often evolved in isolation and designed to meet the needs of the context that they have been developed in. For example, data about medical conditions and medical tests are typically kept at the hospital, data about physical fitness and wellbeing is captured by wearables and mobile apps and stored by 3rd party platforms and data about eyesight and dental problems is stored separately in specific systems.
This has resulted in many data integration and interoperability issues making it very difficult to provide a centred approach for health monitoring, risk predictions, preventions and personalised interventions.
The mechanism for the harmonisation and integration of heterogeneous primary and secondary data adopted in iHelp considers a standardised and extensible approach, based on Holistic Health Records (HHRs), whose notion has been initially realised during the CrowdHealth project.
HHRs is a conceptual model that aims at capturing clinical events and laboratory test results, but also properties about lifestyle, social care, personal measurements, environment, social interactions and in general all health determinants that can be relevant for health risk detection and personal healthcare. Such data may be collected or produced by medical operators, by citizens themselves or by automatic sensors.
There is a huge number of alternative standards in the health domain, such as CCR, DICOM, HL7 CDA, HL7 v2, HL7 v3, HL7 FHIR, openEHR, CEN/ISO EN13606, covering clinical information produced by health professionals and exploited by health institutions worldwide for their EHR (Electronic Health Record) systems. Specific health data models have also been defined for representing information used for or produced by medical researchers, such as HCSRN’s Virtual Data Warehouse (VDW) and Observational Medical Outcomes Partnership (OMOP) model. Nevertheless, current standards for integratinγ health records do not completely support the possibility to represent non-clinical events. Also, in the case of clinical information, such as received medical treatments and diagnosis, current models do not allow correctly distinguishing information recorded by the patient from information recorded by the health organization (for most medical data it is assumed that they are recorded from a health organization). Furthermore, several standards are mainly focused on data exchange, while the HHR model also supports data integration and analyses.
 The Holistic Health Record has been defined to address the aforementioned issues. HHR is not a completely new model aiming at replacing the existing health data standards with another more complete one, but it is built on top of existing standards aiming at overcoming some of their limitations. The HHR model is exactly the conceptual model of a FHIR profile. FHIR defines a logical schema, as its data structure depends on REST architecture features, and a FHIR profile consists of a set of constraints and extensions on this logical schema, thus generating another and more specific logical schema. Being independent of specific implementation architectures, the HHR model is rather a conceptual schema which, although compliant to FHIR, can also be used independently from FHIR. Therefore, the HHR representation allows the creation of different physical models for the same type of data. A software system adopting the HHR model could use, for instance, a FHIR implementation as an in-memory or persistence models, as well as alternative implementations that could better satisfy the requirements of the context in which it is used (e.g. mobile apps or research application requiring less verbose serializations). Additionally, a FHIR profile does not have a standard visual representation, whilst the HHR conceptual model has an UML representation, making it understandable even to people with no experience on FHIR.
The Holistic Health Record has been defined to address the aforementioned issues. HHR is not a completely new model aiming at replacing the existing health data standards with another more complete one, but it is built on top of existing standards aiming at overcoming some of their limitations. The HHR model is exactly the conceptual model of a FHIR profile. FHIR defines a logical schema, as its data structure depends on REST architecture features, and a FHIR profile consists of a set of constraints and extensions on this logical schema, thus generating another and more specific logical schema. Being independent of specific implementation architectures, the HHR model is rather a conceptual schema which, although compliant to FHIR, can also be used independently from FHIR. Therefore, the HHR representation allows the creation of different physical models for the same type of data. A software system adopting the HHR model could use, for instance, a FHIR implementation as an in-memory or persistence models, as well as alternative implementations that could better satisfy the requirements of the context in which it is used (e.g. mobile apps or research application requiring less verbose serializations). Additionally, a FHIR profile does not have a standard visual representation, whilst the HHR conceptual model has an UML representation, making it understandable even to people with no experience on FHIR.
The data model, implemented following the HHR definitions, will be the primary data storage format in the iHelp big data platform. The development of HHRs in iHelp will incorporate metadata structures capturing and enriching the main health record attributes, also extending to behavioural, lifestyle, nutrition, genomics and social properties. Moreover, rules will be developed to automatically establish correlations between different parameters in the HHR structure, to allow new data parameters (e.g. data fields made available through a new diagnostic technique or wearable device) to be added with time.